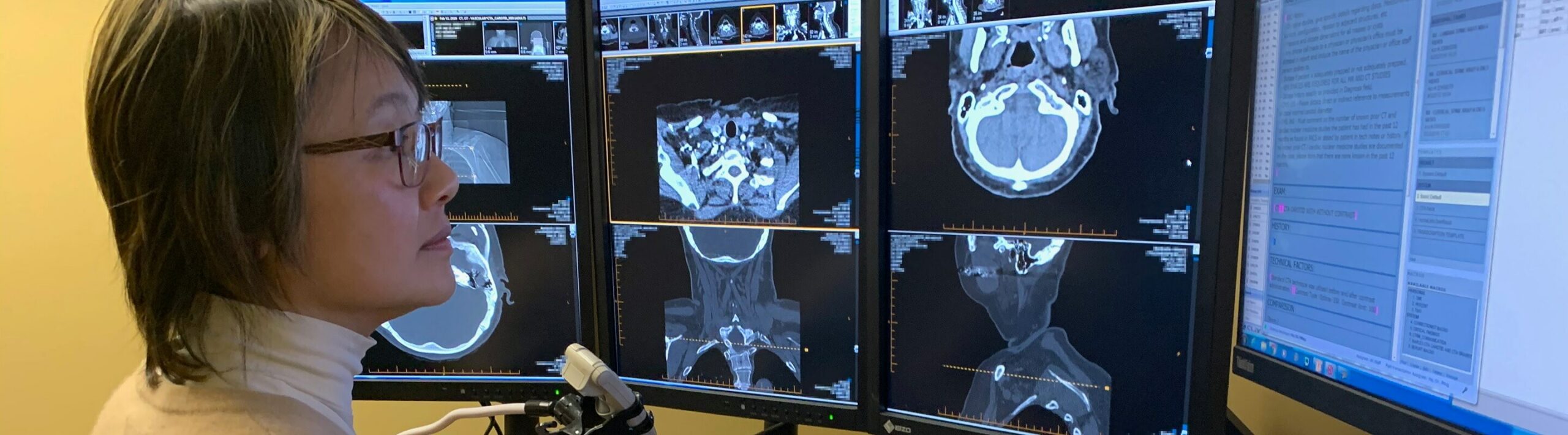
Teleradiology Services
ProScan’s radiology team of fellowship and subspecialty trained radiologists provide expert interpretations for every modality, including MRI, CT, PET, and Ultrasound. We are your dedicated teleradiology partner and offer a streamlined process with easy connectivity, around-the-clock support, and report access through our proprietary, HIPAA-compliant, user-friendly ProScan Online portal.

Our expertise includes:
- Cardiac
- Neuroradiology
- MSK including feet, ankles, elbows, hands
- Chiropractic
- Breast Imaging/3D Imaging
- Prostate
- Body
Discover ProScan Reading Services
Learn more about how to put our expert teleradiology services to work at your practice. Fill out the form below, and we'll be in touch!

Judith M. Turner
Vice President of Sales, ProScan Reading Services
513.604.9231 / jturner@proscan.com
See the ProScan Reading Services Difference
We’re your partner with comprehensive services, technology, staff, and the infrastructure to provide you with the support you need when you need it. A partnership with ProScan Reading Services is the full-service imaging solution your practice needs.
Your Dedicated Teleradiology Partner
-
Subspecialty Reads
-
Over Reads
-
24/7 Best-In-Class Support
-
Online, HIPAA-Compliant Report Access
-
Peer Reviews
-
Vacation Coverage
Tools and Resources
A secure online portal for our radiology partners to submit medical images, upload clinical documentation, and review/deliver patient reports quickly and conveniently.
LEARN MORE
A secure portal for ordering physicians to view medical images easily in a web-based diagnostic viewer and retrieve patient radiology reports – 24/7.
LEARN MORE
Recognized for Excellence by the AAOE
In a 2021 Peer Review survey by The American Association of Orthopaedic Executives (AAOE), 100% of respondents strongly agreed (75%) or agreed (25%) that ProScan Reading Services’ Advanced Imaging Radiology Interpretations “exceeded expectations.” And 95% in the same survey would recommend us to colleagues. The AAOE provides advocacy, networking, and business development for the profession of orthopedic and musculoskeletal healthcare.